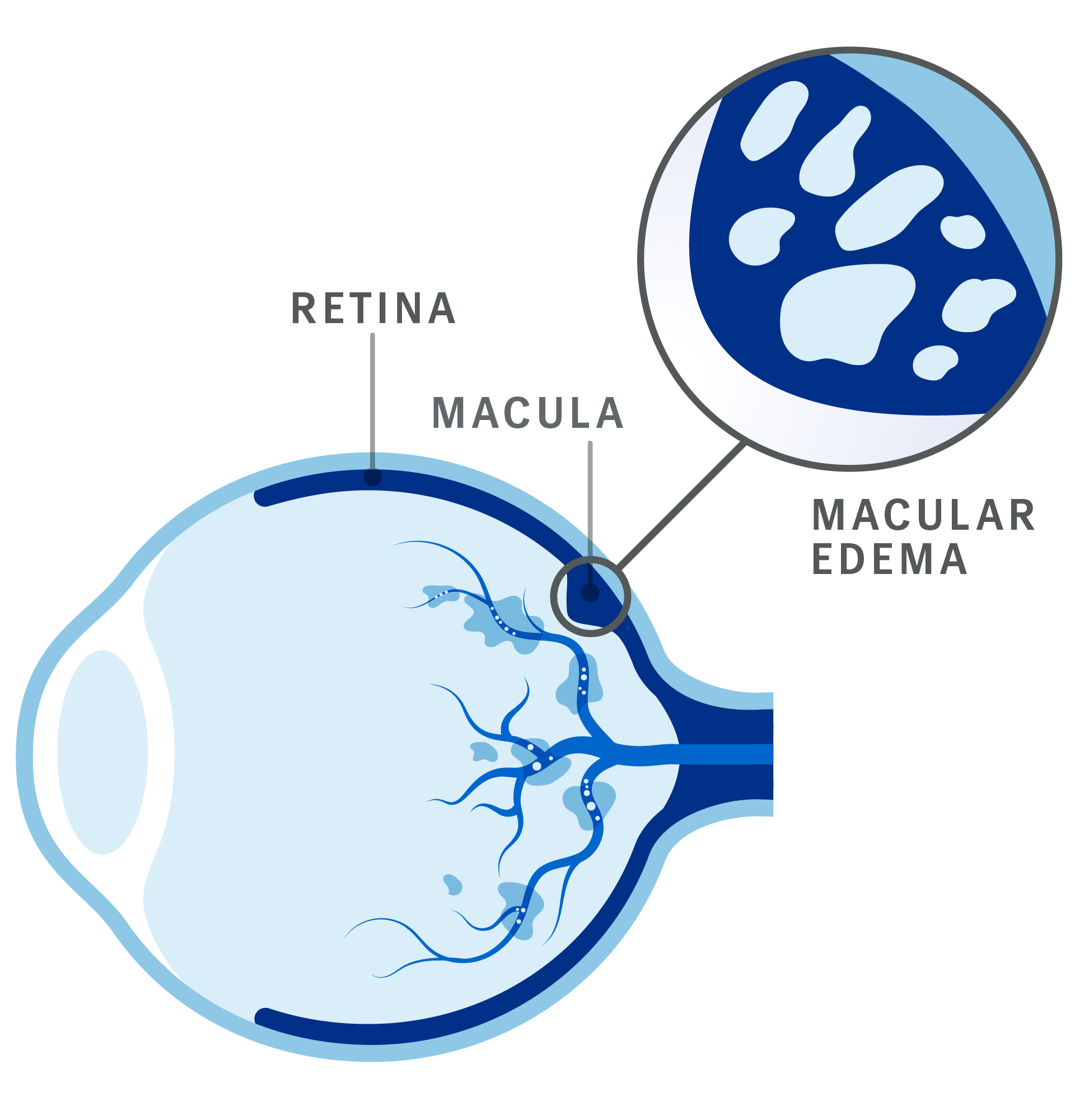
What is DME?
Diabetic macular edema (DME) is a complication of diabetes that can lead to vision loss. In DME, fluid leaks from weakened or damaged blood vessels in the eye and causes buildup in the macula (the central part of the retina which is responsible for clear, sharp vision). This fluid buildup (macular edema), if left untreated, can lead to significant visual damage and make it difficult to see clearly.1,2